Have you ever experienced unexplained bloating, constipation, or diarrhea? While these symptoms are commonly associated with digestive issues, they can also be a sign of a deeper problem: pelvic floor dysfunction. This may sound surprising, but the intricate connection between your pelvic floor and digestive system is more complex than you might think. The pelvic floor, a group of muscles that support your bladder, uterus, and rectum, plays a vital role in regulating bowel function. When these muscles become weakened, tight, or imbalanced, it can lead to a cascade of digestive problems, impacting your overall health and well-being.
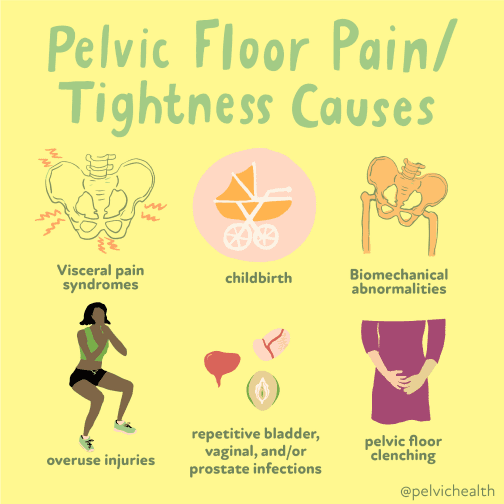
Image: inspiredtherapy.com
Understanding the interplay between your pelvic floor and digestive system is crucial for effective diagnosis and treatment. This article delves into the fascinating world of pelvic floor dysfunction, exploring its causes, symptoms, and the impact it can have on your digestive health. By shedding light on this often-overlooked connection, we hope to empower you with the knowledge you need to address any digestive concerns you may have and seek appropriate medical attention.
What is Pelvic Floor Dysfunction?
The pelvic floor muscles are a hammock-like structure that supports your internal organs, acting as a crucial component of your body’s core. These muscles help control bladder and bowel function, allowing you to hold your urine and stool. They also play a crucial role in sexual function. However, when these muscles become weakened, overactive, or unable to relax properly, it’s known as pelvic floor dysfunction.
Common Causes of Pelvic Floor Dysfunction
Pelvic floor dysfunction can arise from a multitude of factors, including:
- Pregnancy and childbirth: The pressure of a growing uterus and the trauma of vaginal delivery can weaken pelvic floor muscles.
- Age: As we age, muscle strength naturally declines, including the pelvic floor muscles.
- Chronic constipation: Straining during bowel movements can put undue pressure on the pelvic floor, causing weakness over time.
- Obesity: Excess weight can put added pressure on the pelvic floor, contributing to muscle strain.
- Surgery: Pelvic surgeries, particularly those involving the bladder, uterus, or rectum, can sometimes damage pelvic floor muscles.
- Trauma: Injuries to the pelvic region, such as from a car accident, can weaken or damage pelvic floor muscles.
- Neurological conditions: Conditions like multiple sclerosis or stroke can affect nerve function, leading to problems with pelvic floor muscle control.
- Lifestyle factors: Prolonged sitting, smoking, and lack of physical activity can all contribute to pelvic floor weakness.
The Link Between Pelvic Floor Dysfunction and Digestive Problems
The connection between your pelvic floor and digestive system is close and multifaceted. Here’s how pelvic floor dysfunction can lead to digestive problems:

Image: allthenourishingthings.com
1. Constipation and Difficulty Defecating
A weakened pelvic floor can make it difficult to fully empty the bowels. The muscles responsible for pushing stool out of the rectum may not function properly, resulting in constipation and feelings of incomplete emptying. This can also lead to straining during bowel movements, further intensifying the cycle of constipation.
2. Diarrhea and Incontinence
Conversely, an overactive or tight pelvic floor can result in difficulty relaxing the rectal sphincter, making it challenging to control bowel movements. This can lead to accidental stool leakage (fecal incontinence), especially during physical activity, coughing, or sneezing.
3. Bloating and Gas
Pelvic floor dysfunction can also affect how efficiently your digestive tract moves food along. When the muscles are weakened or tight, it can slow down the digestive process, leading to increased gas production and bloating. Poor bowel motility can also contribute to fecal retention, further aggravating these symptoms.
4. Irritable Bowel Syndrome (IBS)
Some researchers believe that pelvic floor dysfunction may be a contributing factor to irritable bowel syndrome (IBS). IBS is characterized by recurrent abdominal pain, bloating, gas, and changes in bowel habits. While the exact cause of IBS is unknown, evidence suggests that pelvic floor dysfunction may play a role in the development and persistence of symptoms.
How to Identify Pelvic Floor Dysfunction
If you experience any of the following symptoms, it may be a sign of pelvic floor dysfunction. It’s crucial to consult a healthcare professional for proper diagnosis and treatment:
- Frequent or urgent need to defecate
- Difficulty emptying your bowels completely
- Straining during bowel movements
- Pain or discomfort during bowel movements
- Accidental stool leakage (fecal incontinence)
- Bloating and gas
- Back pain
- Pelvic pressure
Diagnosis and Treatment
Diagnosing pelvic floor dysfunction involves a combination of medical history, physical examination, and possibly additional tests. Your healthcare provider may conduct a pelvic floor muscle assessment, which involves assessing the strength, tone, and coordination of your pelvic floor muscles. Other tests, such as a rectal examination, colonoscopy, or imaging studies, may be necessary to rule out other underlying conditions.
The treatment for pelvic floor dysfunction will depend on the underlying cause and the severity of your symptoms. Common treatment options include:
1. Pelvic Floor Muscle Exercises (Kegels)
Kegel exercises are effective in strengthening and toning the pelvic floor muscles. Your healthcare provider or physical therapist can teach you the proper technique. Regular Kegel exercises can improve control over bowel movements, reduce incontinence, and alleviate bloating and discomfort.
2. Biofeedback
Biofeedback therapy uses sensors to measure muscle activity and provide real-time feedback. This allows you to learn how to relax and contract your pelvic floor muscles effectively.
3. Electrical Stimulation
Electrical stimulation involves applying gentle electrical impulses to the pelvic floor muscles to help them contract and strengthen.
4. Manual Therapy
A physical therapist or other healthcare provider can use manual techniques to release tension and improve mobility in the pelvic floor muscles. This might involve massage, stretching, or trigger point therapy.
5. Medications
In some cases, medications may be prescribed to address symptoms such as constipation, diarrhea, or pain.
6. Lifestyle Modifications
Making lifestyle changes can also help manage pelvic floor dysfunction and associated digestive problems. These include:
- Maintain a healthy weight: Losing excess weight can reduce the pressure on your pelvic floor muscles.
- Eat a high-fiber diet: Fiber helps regulate bowel movements and prevents constipation.
- Stay hydrated: Drinking plenty of water helps keep your stool soft and easy to pass.
- Avoid smoking: Smoking can weaken muscles, including your pelvic floor.
- Engage in regular exercise: Physical activity can strengthen and tone your pelvic floor muscles.
Can Pelvic Floor Dysfunction Cause Digestive Problems
Conclusion
Pelvic floor dysfunction can manifest in a variety of ways, including digestive problems. Understanding the complex interplay between your pelvic floor and digestive system is crucial for achieving optimal digestive health. If you are experiencing any symptoms of pelvic floor dysfunction, seek medical attention for proper diagnosis and treatment. With early intervention, appropriate treatment options like pelvic floor exercises, biofeedback therapy, and lifestyle modifications can alleviate symptoms and improve your quality of life.





